Memahami Set infusi Komponen dan Asas Keselamatan
Jenis Set Infus dan Kegunaan Perubatan Mereka
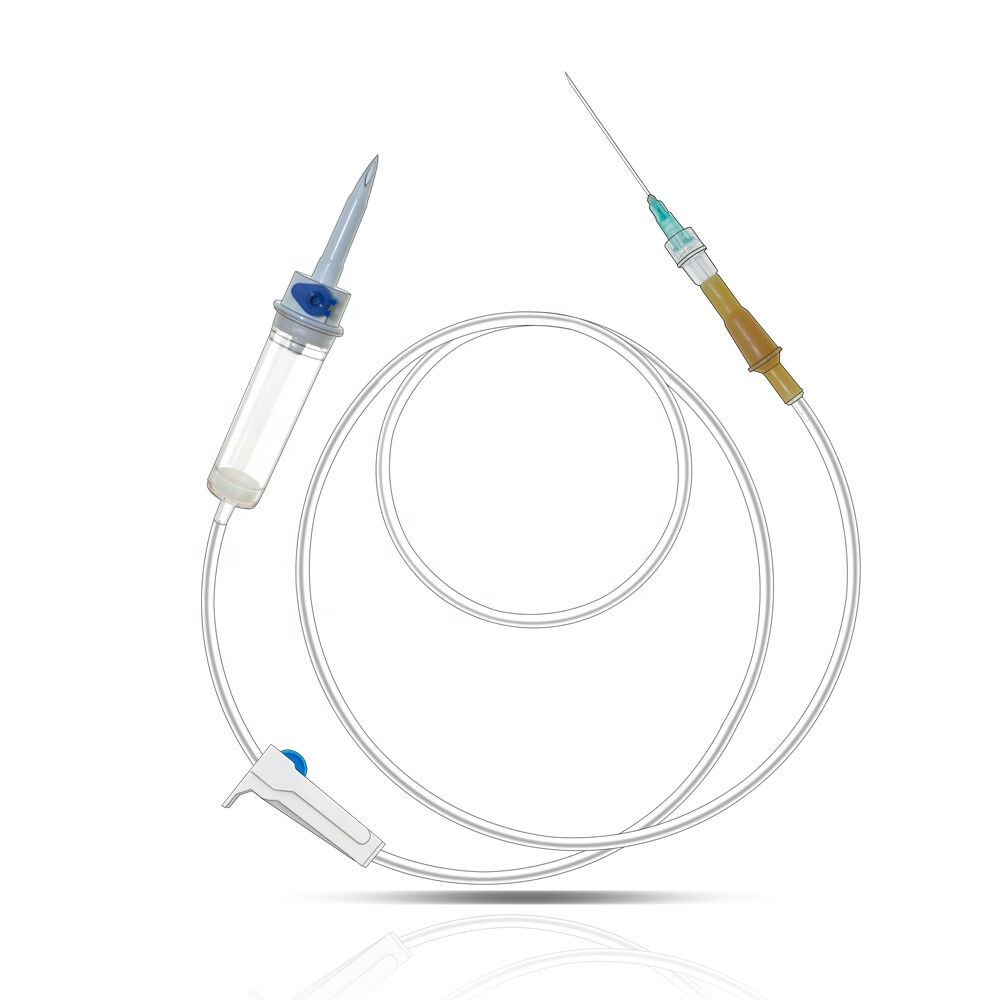
Memahami jenis-jenis set infus dan kegunaannya adalah perkara penting untuk rawatan perubatan yang berkesan. Set infus bervariasi mengikut reka bentuk dan fungsi, termasuklah set infus lurus, sudut, dan keselamatan, setiap satu direkabentuk untuk keperluan perubatan tertentu. Sebagai contoh, set infus lurus biasanya digunakan untuk terapi IV, manakala set sudut menawarkan sudut penyulitan yang lebih mudah pada kawasan di mana set lurus mungkin tidak dapat mencapai dengan mudah. Set infus keselamatan direkabentuk untuk meminimumkan cedera jarum suntik, menjadikannya sesuai untuk situasi di mana keselamatan adalah utama. Set ini memainkan peranan besar dalam pengurusan diabetes, di mana penghantaran insulin adalah berterusan, dan dalam terapi IV untuk pengecaman, yang penting dalam tetapan hospital untuk pengurusan cecair. Memilih jenis yang betul adalah penting berdasarkan keperluan pasien dan jenis ubat, memastikan hasil terapeutik optimum dan mengurangkan komplikasi yang mungkin berlaku.
Kekeliruan Utama Keselamatan bagi Penggunaan Set Infus
Penggunaan set infus yang tidak betul boleh membawa kepada risiko kesihatan yang serius, menegaskan keperluan teknik penerapan yang betul. Risiko termasuk infeksi, trombosis, dan tindak balas tapak, yang kerap berkaitan dengan amalan penyisapan yang buruk. Gejala komplikasi boleh muncul sebagai sakit tempatan, bengkak, atau kemerahan di sekeliling tapak penyisapan, menunjukkan isu potensial. Penyelidikan menekankan keperluan amalan selamat; contohnya, satu kajian di hospital pengajaran mendapati bahawa penanganan yang tidak betul menyebabkan kadar tinggi tiada pembilasan selepas infus, menyumbang kepada hasil negatif kepada pasien. Statistik menunjukkan bahawa sehingga 21% dos antibiotik terbuang disebabkan oleh pembilasan yang tidak betul, menambah kepada kepentingan penggunaan yang betul (Harding et al., 2020). Memastikan amalan selamat boleh mengelakkan komplikasi ini, melindungi kesihatan pasien.
Protokol Pembersihan dan Sterilisasi Perlu
Pensterilan dan higiene adalah perkara utama dalam mencegah pencemaran semasa menangani set infus. Sebelum digunakan, set infus mesti melalui proses pensterilan yang menyeluruh untuk membasmi sebarang pencemar yang mungkin ada. Ini termasuk menggunakan teknik pensterilan yang sesuai untuk memastikan tahap keselamatan tertinggi. Protokol higien, seperti kaedah mencuci tangan yang betul, serta penggunaan kertas penyeka antiseptik, lebih menekankan langkah-langkah keselamatan. Garis panduan dari organisasi kesihatan berkuasa menonjolkan kepentingan protokol ini; mengikut Institut Kebangsaan bagi Kesihatan dan Perubatan Cemerlang, ia adalah asas kepada pencapaian rawatan pasien yang baik dan pencegahan penyakit. Mengikuti protokol ini tidak hanya membantu mengekalkan kesterilan set infus tetapi juga meminimumkan risiko penyakit kepada pesakit yang menerima terapi intravena, menunjukkan kepentingannya yang kritikal dalam persekitaran klinikal.
Panduan Langkah demi Langkah untuk Penyediaan Set Infus dengan Betul
Mengumpul Pasokan Perlu: Senarai Semak untuk Pemula
Memulakan proses dengan senarai semak penuh memastikan persediaan set infus yang betul. Berikut adalah senarai komprehensif untuk memulakan penyiapan anda:
1. Set infus, baik lurus dan bersudut.
2. Ubat-ubatan khas mengikut keperluan pasien.
3. Siring untuk dos yang tepat.
4. Penutup luka untuk mengekalkan tapak infus dan mencegah infeksi.
5. Kapas alkohol dan kain antiseptik untuk mengekalkan kesterilan.
6. Beg untuk pembuangan selamat bahan yang telah digunakan.
Memiliki semua bekalan dalam jangkaun tangan mempermudah proses persediaan dan meningkatkan kecekapan. Persediaan yang betul boleh membuat perbezaan yang besar dalam keselamatan pasien dan kelajuan operasi.
Higien Tangan yang Betul dan Penyediaan Ruang Kerja
Mencipta ruang kerja yang bersih dan teratur adalah perkara penting untuk mengelakkan pencemaran semasa penyediaan set infus. Higien kawalan tangan yang betul juga sama pentingnya dan melibatkan membasuh tangan dengan sabun selama sekurang-kurangnya 20 saat sebelum memulakan prosedur. Kajian daripada Jurnal Kawalan Penjalaran Amerika menekankan penurunan kadar jangkitan dengan protokol kebersihan yang ketat. Untuk membaiki sanitasi, disinfektan permukaan harus digunakan untuk membersihkan ruang kerja daripada pencemar potensial, menyokong persekitaran yang steril.
Penyuaian Saluran Infus: Mengelakkan Risiko Emboli Udara
Pemberian air pada saluran infus adalah langkah kritikal dalam memastikan keselamatan pasien dengan mencegah embolisme udara. Proses ini melibatkan pengisian saluran dengan larutan untuk mengelakkan masuknya kantung udara ke dalam sistem. Langkah-langkahnya termasuk menyambungkan saluran, membuka klip, dan membenarkan cecairan untuk membuang gelembung udara. Pendapat pakar menonjolkan bahaya embolisme udara, seperti peristiwa vaskular bencana, yang menekankan kepentingan pemberian air secara teliti. Menggunakan teknik yang betul tidak hanya melindungi pasien tetapi juga memastikan operasi set infus yang cekap dan selamat.
Teknik Penyelaman Selamat untuk Set Infus
Memilih dan Menyediakan Tempat Penyuntikan
Memilih lokasi suntikan yang tepat adalah perkara penting untuk terapi infus yang berjaya. Faktor yang mempengaruhi pemilihan lokasi termasuk umur pesakit, keadaan urat nadir, dan tempoh terapi. Sebagai contoh, pesakit yang lebih muda atau mereka yang mempunyai urat nadir rapuh mungkin memerlukan pertimbangan lokasi yang berbeza berbanding dewasa dengan urat nadir yang kuat. Untuk memastikan kesterilan dan mengurangkan risiko infeksi, sangat penting untuk membersihkan lokasi yang dipilih dengan teliti menggunakan ejen antiseptik. Jurnal perubatan sentiasa menegaskan bahawa pemilihan lokasi dan persiapan yang betul meningkatkan hasil infus, mengurangkan komplikasi.
Menyemak Kanan: Praktik Terbaik untuk Ketahanan
Memastikan cannula diperbaiki dengan betul adalah perkara penting untuk mengelakkan sesaran dan meminimumkan iritasi. Teknik seperti menggunakan dressing transparen atau tape adhesif boleh menjaga cannula tetap pada tempatnya sambil menyediakan kelihatan kepada tapak penyelitan. Apabila memilih adhesif, pertimbangkan kedua-dua keberkesanan dan keselesaan pasien, dengan memilih pilihan hipoolergenik untuk mengurangkan tindak balas kulit. Garis panduan klinikal menyarankan untuk menyimpan tapak itu kering dan memeriksa tanda-tanda infeksi secara berkala untuk memastikan amalan terbaik diikuti.
Menguruskan Saluran IV untuk Mengelakkan Pengecutan/Pemutusan
Untuk mengelakkan penekukan dan pautan terputus, ia amat penting untuk dengan teliti memosisikan dan meroutkan paip IV. Paip sebaiknya diletakkan di sepanjang anggota badan atau torzo pesakit, mengelakkan kawasan pergerakan kerap yang boleh menyebabkan putaran atau tarikan. Alat seperti penjepit paip atau pengatur boleh membantu mengekalkan kedudukan yang dikehendaki, meminimumkan pergerakan. Kajian menunjukkan bahawa pengurusan paip yang tidak betul membawa kepada bilangan komplikasi yang signifikan, termasuk ralat infus meningkat dan ketidakselesaan pesakit. Oleh itu, pengurusan yang memadai adalah kritikal untuk rawatan yang selamat dan cekap.
Protokol Keselamatan Pemberian Ubatan
Mengesahkan Keserasian Ubatan dengan Set Infus
Pengesahan keserasian ubat dengan set infus adalah perkara penting untuk mengelakkan tindak balas negatif. Profesional perubatan biasanya merujuk carta dan pangkalan data keserasian, seperti Micromedex atau Clinical Pharmacology, untuk memastikan pentadbiran yang selamat. Menurut kajian, ralat ubat akibat ketiadaan keserasian boleh meningkatkan risiko kepada pasien secara signifikan, menjadikan pemeriksaan ini tidak tertawar. Statistik menunjukkan bahawa pemeriksaan keserasian yang tepat boleh mengurangkan ralat ubat sehingga 30%, menonjolkan kepentingan untuk menyertakan langkah ini dalam protokol piawai.
Mengira kadar aliran yang tepat untuk terapi IV
Mengira kadar aliran yang tepat untuk rawatan IV adalah asas kepada rawatan yang berkesan. Formula asas melibatkan pembahagian jumlah isipadu infus dengan masa dalam jam untuk mendapatkan kadar aliran dalam mL setiap jam. Memastikan kejituan adalah kritikal, kerana ralat kadar aliran boleh menyebabkan pelampauan atau kurangnya infus. Ralat biasa seperti pengiraan masa yang salah atau melupakan faktor peralatan seperti penutupan boleh menyumbang kepada ketidaktepatan. Garis panduan klinikal menekankan perhatian teliti terhadap butir-butir ini untuk mengelakkan komplikasi.
Melaksanakan Sistem Pemeriksaan Dua Kali untuk Ubat Berisiko Tinggi
Pelaksanaan sistem pemeriksaan dua kali untuk ubat-ubatan berisiko tinggi boleh meningkatkan keselamatan pasien secara signifikan. Pendekatan ini melibatkan dua profesional perubatan secara bebas memeriksa semula pesanan ubat, pengiraan, dan pentadbiran. Menubuhkan sistem pemeriksaan dua kali yang dapat dipercayai melibatkan protokol yang jelas dan latihan untuk memastikan pemahaman dan ketaatan. Contoh dunia nyata, seperti dari Institut untuk Amalan Pengurusan Ubat Selamat, menunjukkan bagaimana pemeriksaan dua kali telah mencegah ralat ubat dan memperbaiki keputusan. Sistem seperti itu sangat penting untuk ubat-ubatan berisiko tinggi seperti antikoagulan dan kemoterapi, di mana ralat boleh membawa akibat yang serius.
Pemantauan dan Pemeliharaan Semasa Penyedutan
Mengenali Tanda Awal Infiltrasi/Flebitis
Komplikasi berkaitan infus, seperti infiltrasi dan flebitis, memerlukan perhatian segera untuk mengelakkan kesan yang teruk. Infiltrasi berlaku apabila cecairan IV meresap ke dalam jaringan sekeliling, manakala flebitis adalah peradangan pada urat nadi. Tanda awal termasuk pembengkakan, kemerahan, dan sakit di tapak infus. Untuk memantau semasa infus, profesional perubatan harus menyemak secara rutin kepada perubahan suhu kulit dan tekstur di sekitar tapak suntikan. Senarai semak yang merangkumi gejala ini boleh membantu dalam pengesanan awal, memastikan campur tangan awal. Menurut penyelidikan, kadar kejadian infiltrasi berkisar antara 23% hingga 70%, menekankan keperluan pemantauan teliti untuk membaiki hasil pasien.
Protokol untuk Pembersihan Laluan Secara Rutin dan Perubahan Kain Penutup
Pembersihan saluran secara rutin dan perubahan dressing adalah amalan penting untuk mengekalkan keterbukaan IV dan mengelakkan infeksi berkaitan kateter. Menetapkan jadual untuk aktiviti ini memastikan bahawa saluran kekal bersih dan steril. Dianjurkan untuk mengikuti rutin di mana saluran dibilas dengan larutan saline sebelum dan selepas pemberian ubat, sekurang-kurangnya setiap 8 jam, atau mengikut panduan institusi. Penggunaan sarung tangan steril dan lap alkohol semasa perubahan dressing boleh mengurangkan risiko infeksi secara signifikan. Panduan am terbaik dari badan berkuasa, seperti Centers for Disease Control and Prevention (CDC), menekankan kepentingan protokol ini untuk memastikan keselamatan pasien dan terapi infus yang cekap.
Kebutuhan Dokumentasi untuk Terapi IV Berterusan
Dokumentasi yang tepat adalah perkara penting dalam rawatan IV berterusan untuk mengekalkan rekod rawatan yang jelas dan memastikan keselamatan pasien. Unsur utama dokumentasi termasuk jenis larutan, kadar infus, dan sebarang komplikasi yang diperhatikan semasa rawatan. Baik rekod elektronik mahupun kertas memainkan peranan masing-masing; bagaimanapun, dokumentasi elektronik semakin dipilih kerana kemudahannya untuk diakses dan dikaitkan dengan sistem data pasien lain. Menurut kajian, dokumentasi yang menyeluruh berkaitan erat dengan peningkatan keputusan pasien, kerana ia memudahkan komunikasi yang tepat di kalangan penyedia rawatan kesihatan, mengurangkan ralat ubat dan meningkatkan kualiti rawatan secara keseluruhan.
Penyelesaian Masalah Komplikasi Set Infus Biasa
Menguruskan Penutupan Tanpa Mengompromi Steriliti
Penutupan adalah penyumbatan yang berlaku dalam set infus, menyebabkan gangguan dalam penghantaran cecair. Untuk menguruskan penutupan dengan efektif tanpa menjejaskan kesterilan, penting untuk menggunakan teknik steril, seperti menggunakan permukaan bersih dan tangan yang telah disterilkan semasa menangani penutupan. Berikut adalah langkah-langkah yang boleh anda ikuti:
1. Tentukan sebab penyumbatan dengan memeriksa paip untuk lipatan atau kotoran.
2. Siram saluran secara perlahan dengan larutan saline untuk membersihkan sebarang halangan.
3. Jika penyumbatan masih wujud, gantikan set infus dengan segera untuk mengembalikan aliran yang betul.
Kajian menunjukkan bahawa ketaatannya kepada protokol aseptik yang ketat secara signifikan meminimumkan risiko infeksi semasa penyelesaian penutupan (Renard et al., 2010). Pendekatan proaktif ini tidak hanya menyelesaikan penutupan tetapi juga memastikan keselamatan persekitaran terapeutik.
Menyiasat Tindak Balas Alergi atau Ekstravasasi
Tindak balas alergi dan ekstravasasi adalah komplikasi yang mungkin berlaku semasa rawatan infus. Tindak balas alergi boleh memperlihatkan ruam, gatal, atau bengkak di sekitar tempat infus, manakala ekstravasasi melibatkan pengecutan cecair ke dalam jaringan bersebelahan, menyebabkan sakit atau bengkak. Dalam kes seperti ini:
1. Henti infus dengan serta-merta dan menilai pasien untuk mana-mana gejala yang bertambah buruk.
2. Berikan antihistamin bagi tindak balas alergi, atau letakkan kompres suam untuk ekstravasasi.
3. Pemberitahuan penyedia perubatan dengan segera untuk penilaian dan campur tangan lanjut.
Pedoman dari Persatuan Farmasi Sistem Kesihatan Amerika menekankan kepentingan pengenalan dan tanggapan segera untuk mengurangkan hasil negatif. Mengikuti protokol yang ditetapkan memastikan keselamatan pasien dan meminimumkan risiko komplikasi abadi dari isu-isu berkaitan infus ini.
Bilakah dan Bagaimana Menukar Kelengkapan yang Tidak Berfungsi
Pengenalan bilamana untuk menggantikan peralatan set infus yang rosak adalah kritikal untuk terapi tanpa gangguan. Tanda-tanda yang menunjukkan bahawa penggantian diperlukan termasuk keadaan gula darah tinggi yang berterusan dan tidak dapat dijelaskan serta isyarat alarm pom yang menunjukkan masalah dalam penghantaran. Untuk menggantikan bahagian yang rosak dengan selamat:
1. Sediakan kawasan kerja yang steril dan kumpulkan bekalan yang diperlukan.
2. Keluarkan set sedia ada dengan lembut, memastikan gangguan minimum.
3. Masukkan satu set baru menggunakan teknik yang disyorkan untuk mengelakkan gelembung udara atau lipatan pada paip.
Mengabaikan isu-isu peralatan boleh menyebabkan kecekapan rawatan terjejas dan ketidakselesaan pasien. Sebagai contoh, kegagalan berterusan boleh menyebabkan tempoh panjang aras gula darah yang tidak terkawal, yang memberi kesan negatif kepada kesihatan keseluruhan. Oleh itu, pemantauan rutin dan penggantian tepat masa komponen infus adalah aspek penting dalam pengurusan infus yang efektif.
FAQ
Apakah jenis-jenis utama set infus yang digunakan dalam rawatan perubatan?
Set infus termasuk set infus lurus, sudut, dan keselamatan, setiap satu direka untuk aplikasi perubatan tertentu seperti terapi IV dan penghantaran insulin.
Bagaimana penggunaan yang tidak betul bagi set infus boleh mempengaruhi kesihatan pasien?
Penggunaan yang tidak betul boleh menyebabkan infeksi, trombosis, dan tindak balas tapak akibat amalan penyisapan yang buruk, mengompromit keselamatan pasien.
Mengapa pensterilan penting bagi set infus?
Pensterilan menghapuskan pencemar potensial, mengurangkan risiko infeksi dan memastikan keselamatan pasien yang menerima terapi intravena.
Bagaimana anda boleh mengelakkan embolisme udara semasa terapi infus?
Memeriksa saluran infus dengan betul dengan mengisiinya dengan larutan sebelum digunakan mengelakkan embolisme udara dan mengelakkan pemasukan gelembung udara ke dalam sistem.