Understanding Infusion Sets and Their Importance
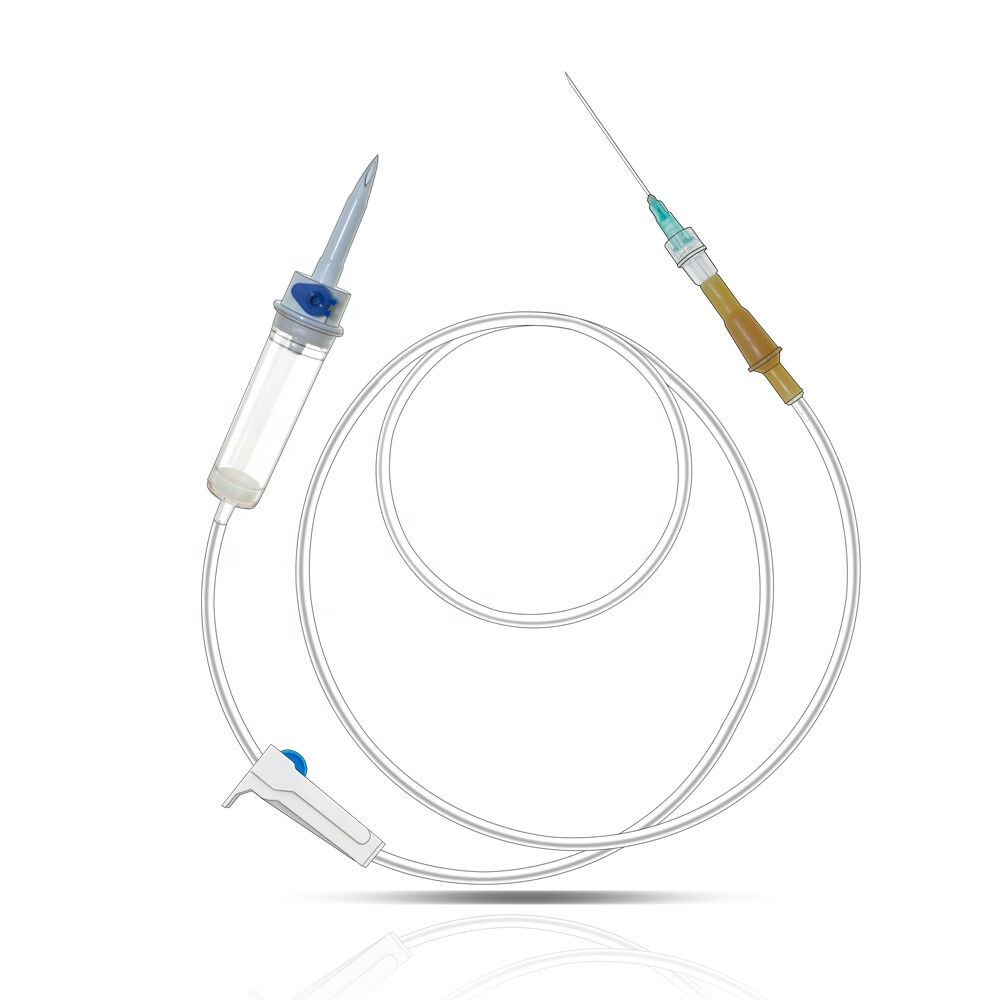
An infusion set is a vital medical device used to deliver insulin to diabetic patients, playing a critical role in the management of diabetes. Infusion sets are generally used with insulin pumps to efficiently and precisely administer insulin, replicating the natural process of insulin release by the pancreas. This device consists of several components, including the cannula, tubing, and connector, all integral to ensuring proper insulin delivery.
The significance of infusion sets in diabetes management is underscored by their role in maintaining optimal blood glucose levels. Proper insulin administration through infusion sets can significantly improve patient health outcomes. For instance, studies indicate that the precise delivery of insulin using these devices can lower the risk of diabetes-related complications. By stabilizing blood sugar levels, patients can experience enhanced quality of life and reduced risk of long-term health issues commonly associated with diabetes, such as nerve damage and cardiovascular diseases.
How to Choose the Right Infusion Set
Choosing the right infusion set is crucial for optimal diabetes management and depends on various factors such as patient age, the type of insulin used, and lifestyle requirements. Patients' age can influence the type of set that is most suitable, as younger users might have different comfort levels or skin sensitivity. Additionally, the kind of insulin and delivery system can affect the choice. For instance, rapid-acting insulin may require a set with a short cannula to facilitate quicker absorption. Lifestyle considerations, such as the level of physical activity, can also dictate the preference for certain types of infusion sets.
Comfort and ease of use are essential aspects to consider, especially for first-time users of infusion sets. The comfort level can significantly affect compliance and overall user experience. Ease of use involves considering whether the set requires manual insertion or if it comes with an insertion device, which can be a deciding factor for individuals who may have dexterity challenges or fear needles. These factors ensure that users do not face unnecessary challenges in their daily management of diabetes, thus enhancing adherence to their treatment regimen.
Infusion sets come in various types, each with specific implications on insulin absorption and patient preference. Common types include straight-in sets, angled sets, and sets with steel needles. Straight-in sets, such as the Quick Set, insert the cannula perpendicularly and are suitable for those with more body surface area. Angled sets offer longer cannulas inserted at an angle, making them preferable for individuals with thin body profiles. On the other hand, steel needle sets, while requiring more frequent changes, mitigate the risk of kinked cannulas and are beneficial for those with scar tissues or who experience frequent occlusions. Understanding these options and their implications allows patients and healthcare providers to customize diabetes management to best fit the patient’s needs.
Comparing Different Infusion Set Options
When comparing infusion sets, it is essential to understand the differences between Teflon and steel cannulas. Teflon cannulas are favored for their flexibility and comfort, as they are designed to bend with the body's movements, reducing site irritation. In contrast, steel cannulas are renowned for their durability and consistent insulin delivery, as they use firm needles that remain securely in place. Each has its own safety profile and patient experiences, making it important for users to choose based on their personal needs and preferences.
Additionally, the method of insertion—manual or automatic—plays a crucial role in the usability of infusion sets. Manual insertion allows users more control, which some find reassuring, although it may require more dexterity and can be uncomfortable. Automatic inserters, on the other hand, are designed for ease of use, providing a quick and consistent technique. According to user testimonials, such automated systems can significantly reduce anxiety associated with insertion. Clinical research has shown that automatic inserters can enhance consistency in the depth and angle of insertion, potentially improving overall comfort and reliability of insulin delivery.
Tips for Effective Infusion Set Usage
Effectively using an infusion set hinges on selecting the appropriate site for insertion. Common infusion sites include the abdominal area, thighs, hips, and the back of the arms. Each site has its own absorption rate. For instance, the abdominal area is often preferred as it offers the most consistent insulin absorption. To ensure optimal insulin delivery, it's important to avoid areas with scar tissue, tattoos, or body piercings, as well as staying away from bony surfaces or spots where tight clothing might constrict the infusion set. Remember, the site should be at least two inches away from the navel.
Maintaining proper hygiene around the infusion site is critical to preventing infections and related complications. Adherence to clinical recommendations is essential for this purpose. Prior to insertion, hands should be washed thoroughly, and the insertion site should be cleaned with soap. Changing the infusion set immediately after a shower can help maintain cleanliness. Even with meticulous care, infections can occasionally occur, so it's vital to recognize early signs like redness, swelling, or pain. Prompt medical attention should be sought to address any infections, ensuring the continued effectiveness of insulin therapy.
Recognizing When to Change Your Infusion Set
Recognizing the signs of an ineffective infusion set is crucial for managing diabetes effectively. Some indicators of ineffective insulin delivery include consistently erratic blood sugar levels and discomfort or irritation at the infusion site. For instance, if blood glucose levels remain unusually high despite proper insulin administration, the infusion set might need changing. Discomfort or redness around the site can also be signs that warrant attention.
It's important to know when to seek medical advice regarding your infusion set. According to expert recommendations, if problems persist after a set change or if there are signs of infection, such as swelling or fever, contacting a healthcare provider is imperative. Delayed changes in the infusion set can lead to serious complications, reinforcing the need for timely intervention to ensure effective insulin therapy and prevent adverse outcomes.
How to Troubleshoot Common Issues
Addressing common issues with infusion sets, such as kinked cannulas and skin reactions, is crucial for effective insulin management. To manage kinked cannulas, it's essential to check the infusion site regularly for unexplained changes in insulin absorption, such as random blood sugar variations. One preventive measure is to use infusion sets with kink-resistant tubing and ensure proper installation without excessive twisting or bending during insertion. Additionally, replacing the infusion set every 2 to 3 days can help prevent kinking.
Managing skin reactions requires a different approach. If you experience irritation, redness, or itching at the infusion site, it’s advisable to rotate sites regularly to minimize stress on the skin. Use hypoallergenic adhesive and ensure the area is clean and dry before insertion. For persistent reactions, over-the-counter hydrocortisone cream can be used sparingly, but it is important to consult a healthcare provider if irritation continues or worsens. They can offer solutions tailored to individual needs, ensuring you maintain optimal comfort and effectiveness in infusion therapy.
Consulting with Healthcare Professionals
Healthcare professionals play a crucial role in guiding patients through the selection and use of infusion sets. Their expertise in diabetes management is invaluable, particularly when it comes to educating patients about the diverse options available. By considering individual lifestyle, health needs, and preferences, they ensure that patients choose the most suitable infusion set. Additionally, healthcare providers can instruct on correct usage techniques, helping to minimize potential complications associated with infusion sets.
Regular follow-ups with healthcare providers are equally important for ongoing support and device management. These appointments allow professionals to troubleshoot any issues that arise with infusion sets and provide personalized recommendations based on the latest medical practices and guidance. Establishing a routine schedule for follow-ups can lead to improved glucose management and help patients maintain better quality of life. Engaging in open communication with healthcare professionals cultivates a supportive environment for successfully managing diabetes with infusion sets.
FAQ
What is an infusion set used for?
An infusion set is used to deliver insulin to diabetic patients, helping in the precise administration of insulin via insulin pumps.
How do I choose the right infusion set?
Consider factors such as patient age, the type of insulin, and lifestyle requirements. Comfort and ease of use are also important.
What are the differences between Teflon and steel cannulas?
Teflon cannulas are flexible and reduce irritation, while steel cannulas are durable and provide consistent insulin delivery.
What common issues might I encounter with an infusion set?
Common issues include kinked cannulas and skin reactions. Regular monitoring and proper site rotation can help manage these issues.
When should I change my infusion set?
Change your set immediately if you experience erratic blood sugar levels or discomfort at the infusion site. Regular changes every 2-3 days are recommended.